The presence of antibodies doesn’t rule out need for COVID-19 vaccine
Aug 11, 2021, 1:48 PM
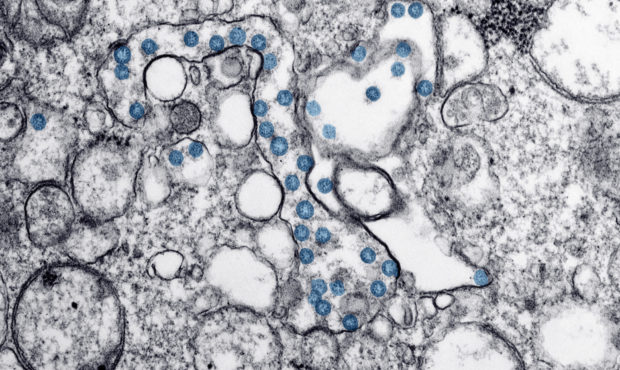
This 2020 electron microscope image made available by the U.S. Centers for Disease Control and Prevention shows the spherical particles of the coronavirus behind COVID-19, colorized blue, from the first U.S. case of COVID-19. Antibody blood tests for the coronavirus could play a key role in deciding whether millions of Americans can safely return to work and school. But public health officials warn that the current “Wild West” of unregulated tests is creating confusion that could ultimately slow the path to recovery. (Hannah A. Bullock, Azaibi Tamin/CDC via AP)
(Hannah A. Bullock, Azaibi Tamin/CDC via AP)
SALT LAKE CITY — Antibody testing in people who’ve had COVID-19 has become almost as common as COVID-19 testing itself. But doctors warn that COVID-19 antibodies shouldn’t determine whether or not to get the COVID-19 vaccine.
Han Kim, a public health professor at Westminster College, said all that antibodies prove is that your immune system responded to a virus it came into contact with.
RELATED: Large antibody study offers hope for virus vaccine efforts
“We don’t even know what level of antibodies are required to fight off COVID,” Kim said, “so, getting an [antibody] test won’t tell you if your immune system will prevent you from getting sick.”
Nicholas Rupp, communications director at the Salt Lake County Department of Health, echoed those sentiments. “The FDA and the CDC are very clear. A positive result from an antibody test does not mean you have a specific amount of protection from infection.”
Kim said he doen’t advise people to get antibody testing for the same reasons. “How many antibodies you need or at what level just isn’t known, yet. So when people ask me if they should be tested to make sure the vaccine took, or if they are protected from a past infection, I’m reluctant to say ‘yes’.”
RELATED: Utah COVID-19 treatment study is in need of more volunteers
Both Rupp and Kim said antibody testing is best used by researchers trying to determine the overall effectiveness of a vaccine in the general populace. Or, how the human immune system responds when exposed to the virus. But they both agreed that individuals should not use these tests to determine if they are protected from COVID-19.
Vaccination and breakthrough cases
Rupp said it’s very important that everyone is vaccinated, even if there’s still a risk of breakthrough infection. A breakthrough infection occurs when someone is fully vaccinated and still test positive for COVID-19.
“The reason some people get sick (after being vaccinated) is that their immune response is not as robust as someone else’s. So they’re more susceptible to infection.”
However, Rupp admitted that the effects of the illness are likely to be lessened in a breakthrough case.
Breakthrough cases and yearly vaccines
Some illnesses like measles only require a one-time inoculation, Kim said, as opposed to the flu which requires yearly vaccines.
He said how well a virus mutates, or changes is the key. “Measles doesn’t replicate well, so it doesn’t change. Whereas influenza is a master at mutating,” said Kim.
SARS, another type of coronavirus, was extremely deadly. “But it’s a bad virus,” Kim said, “because it killed its hosts faster than it could mutate, so we didn’t have a worldwide spread.”
Kim placed COVID-19 somewhere between the measles and the flu in terms of how well it changes. This is why health care officials will most likely recommend yearly vaccinations.
“If there were no variants, if the genetic code never changed, we wouldn’t need annual vaccines,” Kim said.
How To Prevent the Spread of COVID-19 Coronavirus
COVID-19 coronavirus spreads person to person, similar to the common cold and the flu. So, to prevent it from spreading:
- Wash hands frequently and thoroughly, with soap and water, for at least 20 seconds.
- Don’t touch your face.
- Wear a mask to protect yourself and others per CDC recommendations.
- Keep children and those with compromised immune systems away from someone who is coughing or sneezing (in this instance, at least six feet).
- If there is an outbreak near you, practice social distancing (stay at home, instead of going to the movies, sports events, or other activities).
- Get a flu shot.
Local resources
Utah’s Coronavirus Information
The Church of Jesus Christ of Latter-day Saints
Utah Coronavirus Information Line – 1-800-456-7707
National Resources
Centers for Disease Control and Prevention
Commonly asked questions, World Health Organization













